Live poor, die young
Another study -- one that takes government transfers into account -- confirms living in poverty is associated with ill-health and early mortality
Epidemiologists have long noted that people who earn less money live shorter lives and suffer more ill-health than people with more money. One recent study documenting this phenomenon found that “higher income was associated with greater longevity throughout the income distribution.”
That 2016 study, led by Stanford economist Raj Chetty, found the greatest difference in longevity was between people in the bottom and top 1% of the income distribution, where the gap was about 15 years for men and 10 years for women. To put that spread in perspective, the richest 1% lived longer than people in Japan, which is ranked first in longevity, while the poorest 1% lived about as long as the average person in Russia or North Korea, which are tied for 113th.
Just a few months before that study appeared, Anne Case and Angus Deaton, who had just won the Nobel Prize for economics, documented a rapidly falling longevity rate for white Americans. The main causes were “drug and alcohol poisonings, suicide, and chronic liver diseases and cirrhosis,” which they dubbed “deaths of despair.”
Those studies appeared around the time the U.S. entered what has become an unprecedented long-term slide in life expectancy, which was only exacerbated by the COVID pandemic. The latest data show U.S. average life expectancy fell to 76.1 years in 2021 after peaking at 78.9 years in 2014.
In other words, stagnant incomes in the lower half of the income distribution and our bungled response to the pandemic managed to chop nearly three years of life off the average American over the past decade. The average masks huge inequities. Black Americans lost four years over that span; indigenous people more than six years. Both groups include a disproportionate share of the nation’s poor.
Updating the definition of poverty
I was prompted to revisit that literature this week after seeing a brief research note in JAMA Internal Medicine that tried to address some of the criticism leveled at the original JAMA study. This new study also viewed its findings through a health care lens: What would our response to poverty and inequality be if we treated stagnant real income and growing income inequality like a disease?
Before addressing that second question, the authors corrected for what is the most frequent conservative critique of studies that tie deteriorating health for people in the bottom 20-30% of the income distribution to enduring poverty: the impact of safety net programs like child tax credits, the earned income tax credit and food stamps on income.
Conservatives claim poverty is grossly overestimated because the Census Bureau’s calculations do not include the value of transfer payments. For instance, former Sen. Phil Gramm, now at the conservative American Enterprise Institute, estimated in a Wall Street Journal commentary last November that anti-poverty programs funnel a staggering $1.9 trillion a year into the households of the poor (I’d like to know how he arrived at that number given that the entire federal budget for non-defense discretionary spending was only $800 billion in 2022).
David Brady, who’s at the University of California, Riverside, and colleagues took that critique into account by wrapping all tax credits and “near cash” transfers like food stamps into their definition of income. Moreover, they expanded their definition of poverty to go up to half the median income. While progressive economists support that expanded definition of poverty, its use in the study meant more better-off but still lower-income Americans would be in the group being evaluated for the ill health effects of poverty.
And here’s what they found: People living in poverty have a 42% greater chance of premature mortality than people in higher income brackets. If they remained mired in poverty for the ten-year period of the study, premature mortality rose by 71%.
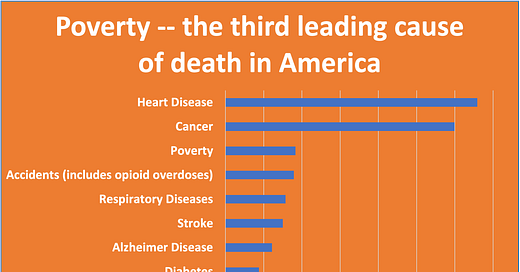
Translated into annual death rates, poverty kills just under 200,000 people per year, making it the third leading cause of death. (If one includes smoking as a cause of death, it falls to fourth. The vast majority of smoking-related deaths are counted as either cancer or heart disease deaths in statistics compiled by the Centers for Disease Control and Prevention.)
President Biden has launched a “moonshot” to cure cancer. The nation’s media, whether aimed at a mass audience or the specialized health care press, run articles and segments almost daily about the untreated high blood pressure, obesity, substance abuse and mental illness that is leading to early mortality and driving down longevity.
Yet we rarely see stories that directly address the fact that poverty and economic stress on low-wage workers is triggering a disproportionate share of those illnesses. Nor do we hear many politicians articulating a program to address what may well be the number one cause of ill-health in our society: the impact of poverty and growing income inequality.
In a commentary on the Chetty study published seven years ago, Nobel laureate Deaton expressed no surprise that the medical mainstream “emphasizes biology, genetic factors, specific diseases, individual behavior, health care, and health insurance” in its approach to improving the overall health of the population and putting America back on the path toward increasing longevity.
“Even if it is true that the fundamental causes of health are social and economic, there is every reason to focus on treatment and health behaviors in a country, even one as rich as the United States, where poverty is intractable and there is little immediate prospect of making the distribution of income more equitable,” he wrote.
For what it’s worth, I still believe change is possible. I only despair when I think about how much of the $4 trillion we spend on health care each year is wasted, and how even much of what gets done, even when useful, amounts to putting a band aid on the cancer of income inequality.
I will be off next week.